There is no better remedy for BPD than attending a Borderline Inpatient treatment Centre. Living with Borderline personality disorder can be sheer hell.
Most of us are to ‘reason’ with our feelings and ‘pull it together’ if need be. However, individuals with BPD who engage in Borderline Inpatient treatment experience intense and unstable emotions that often feel uncontrollable. Often they describe being on an emotional rollercoaster. Extreme mood swings, emotional reactivity (overreacting to minor events, for example) and intense inappropriate anger are common.
They may also feel a deep fear of being alone, rejected and abandoned, leaving them with a sense of inner hollowness and emptiness.
WHAT IS BORDERLINE PERSONALITY DISORDER ANYWAY?
All of us have a personality and character. We all have our unique likes and dislikes, tastes and preferences and ways we deal with others. You may prefer Chinese food over American food, like a sports car better than an SUV or love basketball and dislike football. Friends or family members may share some of your unique tastes, but likely not all of them. Our uniqueness and individuality is related to how we do things. To a large extent, this defines who we are.
A personality is our own unique set of behaviours, attitudes, thoughts and feelings we bring to situations and people consistently over time. Our personality defines us to such a large extent that friends and family members are able to identify and describe is based on our personality. While we may not always be ‘true to ourselves’ and sometimes act in ways that are ‘not like us at all’, we are for the most part consistent and predictable over time.
With borderline personality disorder, you have an intense fear of abandonment or instability, and you may have difficulty tolerating being alone. Yet inappropriate anger, impulsiveness and frequent mood swings may push others away, even though you want to have loving and lasting relationships. Oftentimes it takes Borderline Inpatient treatment programs 90 days to swing the symptoms around. Once the process starts however it can be one of the best and most liberating experiences anyone can have. People successfully completing Borderline Inpatient treatment often describe the relief as feeling like a 20 to shield has been removed.
Their bodies are less tense and their shoulders feel relaxed, something many borderlines have never really felt before. They describe the freedom from distrusting thoughts and the constant need for chaos, drama and second guessing to be Nirvana-like. Mark L Lockwood (BA)(hons)(psy) says that “BPD or borderline personality disorder is relatively easy to treat. It is starting the treatment that can be super-difficult for some people. Denial, resistance and strong defence mechanisms are characteristic of this disorder at the beginning of Borderline inpatient treatment. Once the person has developed an awareness of their condition, and starts to feel some acceptance of it, the journey can be quite amazing for the individual. Freedom from all the stress is definitely worth the journey, every single time and no one should stay stuck with Borderline, even though most people feel for a time feel they have to contend with it forever.
Not anymore, not in 2023 and beyond. Things have changed and so people are changing their diagnosis’s. They are in fact transforming themselves and their persona’s with the right treatment programs.
Borderline Personality and Addiction
Recovering from a mental illness, such as Borderline Personality Disorder (BPD) and an addiction is challenging. It is also beyond common and up to 80 percent of people in inpatient treatment centres today or rehabs are actually boderline BPD, more so than the traditional definition of an addict. By that we mean a person suffering BPD and medicating with drugs, substances or alcohol for example may do well to treat the Borderline personlity disoder which in turn will positively effect their relationship with substances. This is genrally playing it backwards in the medical field today. Normally you treat the substance issues first. Albeit there are many ways to skin a cat and research today is highly limited.
Often individuals with mental illnesses feel isolated, alone and rejected by family and friends. However, family members, friends and other caring individuals can be a tremendous resource in the recovery process. Some of these supportive people are trained mental health professionals. The vast majority, however, are untrained individuals such as spouses, children, siblings, aunts, uncles, parents or the Alcoholics Anonymous (AA) sponsors. Many of these people want to help their loved one but feel ill equipped to deal with the multitude of challenges their loved one faces.
Similarly, many individuals who are recovering from drug addiction and a co-ocurring disorder are also looking for answers to questions about their disorder. Educating oneself about the disorder is an essential step in recovery.
Many people with BPD and addiction ask themselves “Why me?” You may have a sibling, parent or other relative who also has a serious mental illness or an addiction to alcohol or other drugs, and you probably have many relatives who have not been afflicted with a mental illness or addiction.
BPD and addiction have been linked to learned behaviour, psychological factors, exposure to chronic extremes stressors and a genetic vulnerability. This is underscored by the fact that a vast majority of individuals with BPD (about 60 to 80 percent) report a history of physical, emotional or sexual abuse. IT has even been suggested that BPD is an extreme case of post-traumatic stress disorder (PTSD). It should be pointed out, however, that abuse in and of itself does not cause BPD. Rather, it triggers vulnerable individuals’ potential to develop the disorder.
We have found that individuals with BPD consistently make the following three thinking errors: the conviction of basic badness, mistaking a want for a need and the inability to make compromises.
The Conviction of Basic Badness
Feeling that you are fundamentally flawed, bad and inferior may be familiar to you. Often you may think: “If you really get to know me, you won’t like me and will reject me.” Using alcohol and other substances may have given you brief and temporary relief from these negative feelings, but the intense and deep sense of self-loathing returns once you are sober. Thus, individuals who have BPD and a chemical dependency find themselves in an eternal vicious circle: trying to cover up the bad feelings by using substances, but then having the sense of ‘basic badness’ re-affirmed by the substance use and other self-defeating behaviours.
Through Borderline Inpatient treatment you may find yourself becoming aware, in this cycle believing that “I am not worth anything and don’t deserve to be in a relationship with a decent person” and using a substance to temporarily escape this inner sense of emptiness, worthlessness, hopelessness and powerlessness. Based on your personal experience and environment, you started thinking about yourself in negative terms and internalised this belief over time. If so, stop and imagine yourself as a newborn baby. You were not born with a negative sense of self. Nobody is. Logically, you know that nobody is born feeling bad about themselves.
If you suffer from the conviction of basic badness, you may identify with some of the following statements:
Nobody really cares about me.
I am not a worthwhile person.
If you really get to know me, you will reject me.
Deep down inside, I am fundamentally flawed.
I only feel good when I am around other people.
I deserve to be punished.
I don’t deserve anything positive (friends or success, for example).
If I am myself, everybody leaves.
I can’t stand losing a relationship.
Everything positive is coming from others.
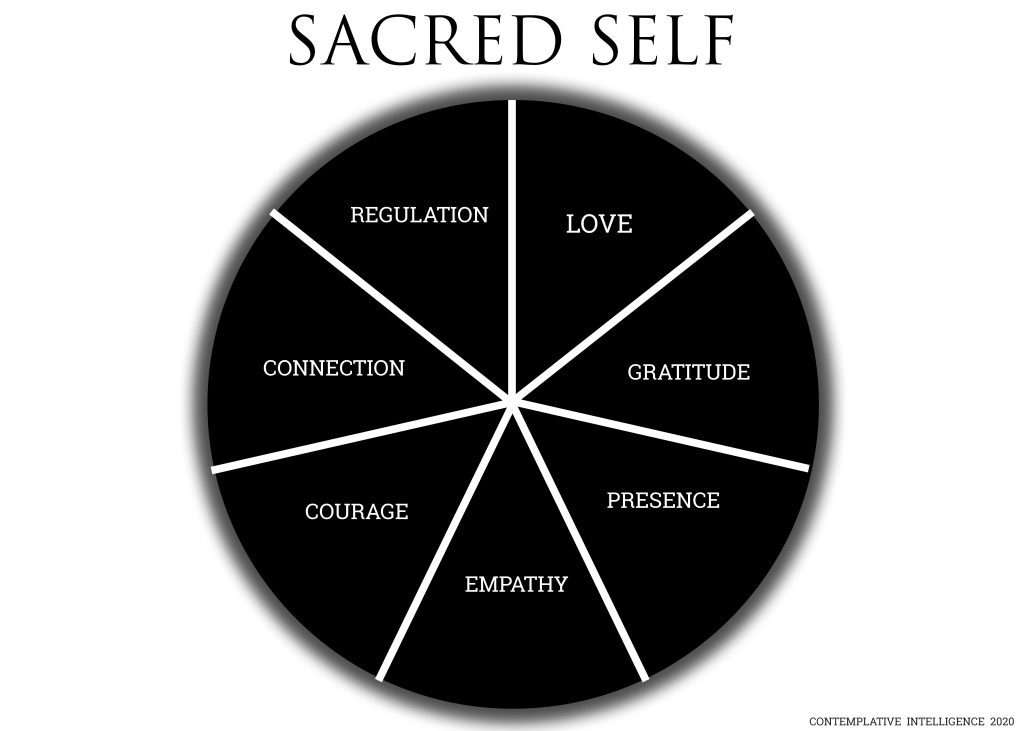
For more information on Borderline Inpatient treatment and the healing experience of a lifetime at our Luxury Wellness and Spiritual healing Centre please call +27824424779 or email info@sanctuaryplett.co.za Our team os psychologists and specialists are ready to welcome you into one of the finest Borderline Inpatient treatment programs in the world. Enjoy everything from our specialised BPD meditation course to the therapy, to the setting and the coursework will help you to find and operate from your Sacred Self.